Vitamin D is not an optional supplement. It is a non-negotiable cellular necessity
From time immemorial, vitamin D has played a vital role in commanding our whole body into a state of wellbeing. The role of vitamin D goes beyond the regulation of calcium and bone health. Low levels of vitamin D can drastically impact a person's physical and mental well being. Vitamin D deficiency has been linked to various health problems, including cognitive decline, depression, osteoporosis, cardiovascular disease, hypertension, diabetes, autoimmune diseases and cancer.
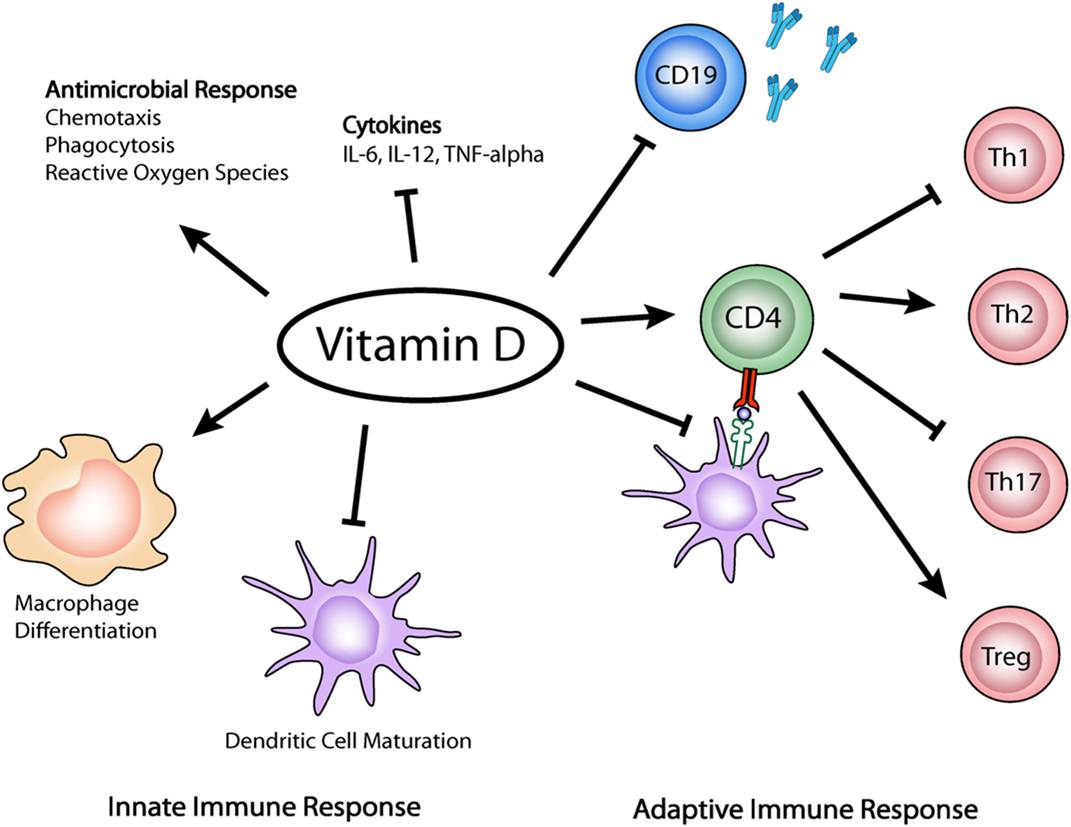
Vitamin D in its active form is actually a master hormone that controls at least 200 genes in our cells. Follwoing the discovery of vitamin D receptors throughout the body, its role in the prevention and treatment of chronic diseases is gaining momentum. It is been positioned as the critical aspect in immune system functioning and gut homeostasis too. It not only offers preventive advantage reducing the probability of contracting some of the most frightening diseases but offers unique therapeutic immune-regulatory role in the treatment of autoimmune diseases.
The successful treatment of auto immune conditions with daily intake of vitamin D has been pioneered by Dr. Cicero Coimbra from Brazil. People with auto-immune diseases usually have various degrees of vitamin D resistance at the cell receptor level. They need higher daily doses of vitamin D as compared to supplemental doses to compensate for the individual level of resistance to the biological effects of vitamin D (including its potent immune modulatory role).
This requires individual tailoring of daily doses according to laboratory results of each patient. My job is to mentor patients on how to discover the best suitable dose of vitamin D, necessary cofactors like magnesium, selenium, zinc, vitamin B2 & B12 along with a low calcium diet rich in liquids. Some autoimmune conditions reverse magically while some come in a state of remission. The aim is to give them the best quality of life without any worsening of symptoms.
Frequently Asked Questions
- How does vitamin D affect autoimmune diseases?
-
- Autoimmune diseases are a result of an unregulated immune system that produces an aberrant immunological Th17 reaction. Vitamin D suppresses autoimmunity by suppressing this Th17 reaction in the immune cells.
- Vitamin D also induces the proliferation of the helpful regulatory immune cells called “T reg” cells that maintain balance in the immune system.
- Vitamin D empowers the immune system against viruses, bacteria, and other microorganisms.
- What is the physiological dose of vitamin D?
-
Human beings of the past were sweating farmers doing manual labor, producing 10 – 20000 units of vitamin D daily with blood levels at 70 – 80 ng/ml, eating fresh food and no artificial calcium supplements. A physiological, safe dose of vitamin D is 10,000 IU/day. The scientific world has accepted that a statistical error was made in calculating the doses for vitamin D. No wonder with such low recommended doses, more than 90 percent of global population is deficit in vitamin D today. The Endocrine Society has indicated that 10,000 IU/day is “NOAEL”- No observed Adverse Effect Level.
- Why do patients with autoimmunity need higher than usual intake of vitamin D?
-
Research disclosed that patients with autoimmune diseases have an increased resistance to the effects of vitamin D. This resistance is mostly due to genetic polymorphisms at the level of the VDR (vitamin D receptors). Consequently, higher than usual doses of vitamin D are needed to overcome this resistance. The dose also depends on the type of autoimmune disorder.
A daily intake of vitamin D in physiological doses or little above, along with pharma-grade magnesium, B2, selenium and omega 3 fatty acids has seen good results in most patients.
Higher doses of vitamin D are needed for few with very high degree of vitamin D resistance.
The doses are subsequently reduced based on the autoimmune disease. - What is the ideal dose of vitamin D for patients with autoimmunity?
-
The dose for each patient would be different. The vitamin D levels cannot be used for dose adjustments. It depends on the degree of vitamin D resistance. The test that evaluates Vitamin D resistance is the degree of drop in PTH (parathyroid hormone) levels. PTH is released by the parathyroid glands and active vitamin D suppresses PTH; consequently, as vitamin D levels go up, PTH levels go down. The aim is to bring the PTH level at its lowest normal limit. When PTH level is at a minimum, the best biological effect of vitamin D is reached for that individual, irrespective of what caused the resistance.
- What are the side effects of this treatment methodology?
-
Vitamin D toxicity is what we are made to be scared of. In reality, vitamin D innocently functions to merely open the doorways in the intestines for proper absorption of calcium to the blood. Its not vitamin D, but the excess calcium that can become toxic! The possible side effect of taking vitamin D for extended periods of time is this excess calcium that reaches wrong places like the blood vessels, kidneys & coronary arteries. If hypercalcemia can be prevented while on therapy, there is no fear of any toxicity. The following steps are taken for the same -
- Ionized calcium levels are monitored periodically to monitor calcium intake through diet.
- PTH levels are periodically monitored and toxicity of vitamin D is rare as long as the PTH levels remain in their range.
- Calcium supplements are stopped as dietary calcium in moderation is enough when well absorbed.
- A diet free of dairy or in moderation (based on the ionized calcium levels in blood) is recommended to ensure the calcium levels are kept under control.
- Addition of vitamin K2-7, to channelize the calcium from the heart and kidney to the bones is advised.
- To avoid loss of bone mass, patients are instructed to practice a daily routine of exercise, like 30 minute fast walk, yoga and pranayam.
- Those who cannot practice aerobic exercise might need medication, such as bisphosphonates.
- How about the kidneys?
-
To keep the kidneys healthy it is fundamental to prevent calcium overload in the body. For that the patient -
- Should commit and take care of the diet as advised
- Should not take calcium supplements randomly.
- Should drink 2.5 L of liquids a day, to ensure that the kidneys eliminate excess calcium.
- Should inform the doctor if they have any history of kidney problems to plan the treatment differently.
- What is the recommended diet on this protocol?
-
Generally, for frequent fish eating patients, dairy and calcium enriched foods must be avoided and nuts should be consumed in moderation. Vegetarian Indians can do with moderate dairy in the form of thin buttermilk and few nuts in general. Again, every patient is different, so the test results will ultimately determine if the diet is being correctly followed or if more restrictions are needed. Water and liquid intake of 2.5 Litres a day is a a must.
- What other supplements are a part of the protocol?
-
To activate vitamin D, magnesium (Chloride / Citrate / Threonate / Glycinate) supplementation is a must. Other supplement requirements vary from patient to patient. They are Riboflavin (B2), Selenium, Omega 3 fatty acids, Zinc….
- How is the treatment monitored?
-
PTH levels are measured regularly during the treatment as achieving the correct functional status of vitamin D accounts for 95% of the treatment. If PTH is not at the lower end of the normal limit, vitamin D daily doses can be increased without any fear. During the treatment, PTH levels are expected to go down to their low normal limit and stay there. When this happens, the resistance to vitamin D is overcome and its powerful effects take over. However, patients start to see the benefits much earlier in most of the cases. It usually takes 6 to 12 months to adjust the dosage. After this period, the treatment is all about maintaining proper levels of PTH and calcium. Some autoimmune diseases need the long term maintenance of vitamin D in higher than normal doses while most continue to remain in remission with just the physiological doses being maintained.
- What are the required lab tests?
-
Some of the tests required for the protocol include, but are not limited to: PTH, Vitamin D3, Ionized calcium, Vitamin B12, Creatinine, Bone Densitometry